Have you ever wondered what really happens inside the brain when Parkinson’s disease strikes?
This article explores the intricate changes within the brain caused by this condition.
Parkinson’s disease is a brain disorder that affects movement functions of the body. People with this disease often have trouble with balance, moving around, stiff muscles, tremors, and shaking. It can also mess with how they talk, stand, and walk. As it gets worse, Parkinson’s can lead to memory problems and other thinking troubles.
The current estimate shows that more than 10 million people worldwide are suffering from this disease, and this number is growing every year. It usually affects men and often starts showing up after they turn 60.
What really happens in the brain that causes Parkinson’s disease?
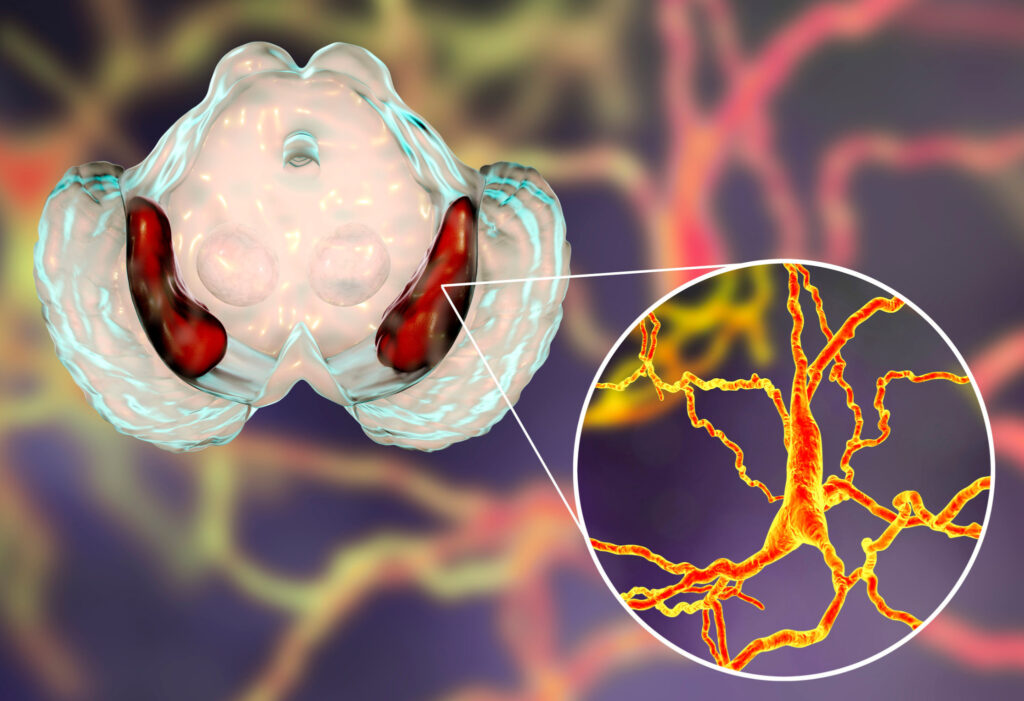
Parkinson’s disease involves various brain changes. However, the primary reason behind its onset is the loss of a specialized group of cells known as dopaminergic neurons. These cells are crucial because they’re responsible for producing dopamine, a vital chemical messenger that regulates movement functions in the brain.
When these cells die, the brain’s ability to produce enough dopamine diminishes. And by the time the typical signs appear, the brain has already lost more than 50% of them. While the exact reasons for the death of dopaminergic neurons remain uncertain, researchers have identified many genetic and environmental factors contributing to this process.
Dopamine has multiple functions in the brain. However, its pivotal role in Parkinson’s disease revolves around controlling movement. To understand this role, we need to dig deeper into the brain and explore the region responsible for its production. This region is called the Substantia nigra, a Latin word meaning black substances. The Substania nigra is itself part of the bigger structure named basal ganglia, which is located deeply in the central part of the brain. Its primary function is to keep the balance in movement, meaning that it regulates when a specific body movement occurs and when it should be restrained.
To understand this balance, imagine how your body remains still as you watch TV, read a book, or even read this article. When you want to move, your brain initiates that action. But when you’re intentionally staying motionless, your brain actively suppresses unintended movements—like sudden head turns or involuntary hand movement. The basal ganglia play a crucial role in controlling these inhibitions. It works by regularly calming the neurons that trigger voluntary movement.
Dopamine from the Substantia nigra plays a key role in releasing this control. However, when there’s a shortage of dopamine due to the death of dopaminergic neurons, the basal ganglia struggle to regulate movement effectively, resulting in difficulties initiating actions. This is why Parkinson’s patients experience difficulty in initiating movement.
What other parts of the brain are affected during Parkinson’s disease?
Initially, the Substantia nigra is the most affected area of the brain in Parkinson’s disease. However, as the disease advances, additional regions within the brain and brainstem are also affected, and they begin to experience cell loss. These areas include the amygdala, hypothalamus, locus coeruleus, and median raphe nucleus. This widespread loss of brain cells across different areas contributes to a range of issues, mainly resulting in the appearance of non-motor symptoms of this disease. These include abnormal sleep, fatigue, constipation, loss of smell, depression, mild memory, and cognitive problems.
What other brain chemicals are involved in Parkinson’s disease?
While dopamine plays a prominent role in Parkinson’s disease, researchers have also identified other brain chemicals that are affected in patients with this condition. One of these is serotonin, often called the “happy chemical” due to its role in boosting well-being and happiness in the brain.
Similar to dopamine, individuals with Parkinson’s experience a drop in serotonin levels. Research indicates a significant decline—up to 50% less serotonin in their brains than those without the condition. Like the reduction in dopamine caused by the loss of dopamine-producing neurons, serotonin faces a comparable fate. Its deficiency is caused by the death of a Substantial number of its producer cells. A point worth mentioning is that while dopamine shortage primarily affects movement, serotonin deficiency in Parkinson’s contributes to both movement-related issues and non-movement challenges experienced by patients.
Glutamate is another brain chemical involved in Parkinson’s disease. It’s a well-known amino acid that functions as a neurotransmitter in the brain. Studies using brain scans and blood tests have revealed higher glutamate levels in the brains and blood of people with Parkinson’s compared to those without the disease. It’s still uncertain whether these changes in glutamate worsen the disease or if they result from the disease progressing. Researchers think that the elevated glutamate levels detected in Parkinson’s might indicate the body’s attempt to compensate for the insufficient dopamine level in the brain.
What physical change appears in the brain during Parkinson’s disease?
Parkinson’s disease involves the loss of cells and their connections in the brain, resulting in a reduction in brain size. The area most affected is often the basal ganglia, which noticeably shrinks in size. As mentioned earlier, the Substantia nigra is located within the basal ganglia and houses neurons that produce dopamine. Normally, the presence of these neurons shows up as black spots due to a pigment called neuromelanin. However, in Parkinson’s disease, the substantial loss of dopamine-producing neurons leads to the disappearance of these black spots. This particular feature, known as the loss of neuromelanin-containing neurons, is a key pathological feature observed in the brains of Parkinson’s patients.
Apart from the basal ganglia, other brain regions that experience a decrease in volume include the thalamus, caudate nucleus, white and gray matter, and various cortical and subcortical areas. Additionally, abnormal structural changes are observed in glial cells, which are non-neuronal cells providing support to neurons in maintaining their structural connections.
How to deal with Parkinson’s disease?
While there’s no cure for Parkinson’s disease, there are medications available that help to manage symptoms and enhance life quality. These medications are formulated to replenish the levels of dopamine in the brain.
Aside from medication, individuals with Parkinson’s should explore additional strategies to manage the symptoms of this disease. These include:
- Engaging in regular exercise
- Maintaining a healthy diet
- Actively participating in social activities
- Seeking out massage therapy and counseling
- Using assistive devices to assist with daily self-care tasks
Related article: The 8 most effective ways of dealing with Parkinson’s disease.
Disclaimer: The information shared here should not be taken as medical advice. The opinions presented here are not intended to treat any health conditions. For your specific medical problem, consult with your healthcare provider.

Make it deeper