Ever wonder how do Parkinson’s medications work?
Parkinson’s medications work by restoring the level of dopamine in the brain. Dopamine is a neurotransmitter that is deficient in the brain of Parkinson’s disease patients. Different classes of drugs are available to treat Parkinson’s symptoms. Although these drugs have different mechanisms of action, their end result is to readjust the brain’s dopamine level.

Parkinson’s disease (PD) is a neurological condition that affects body movements. The disease occurs when a certain group of cells is lost in the brain. These cells are called dopaminergic neurons. When these cells die, the brain cannot release a sufficient amount of dopamine, a neurotransmitter responsible for controlled body movement. As a result, the body shows symptoms like tremor, slowness of movement, rigidity, and balance problems.
Parkinson’s medication’s main aim is to restore the amount of dopamine in the brain. In order to understand better how they do it, we need to look at the way dopamine is produced by the dopaminergic neuron.
The picture below shows the dopaminergic neuron (the presynaptic neuron) on the left side. Here, dopamine is produced in a two-step process. In the first step, the amino acid tyrosine converts into levodopa (also called L-DOPA) with the help of an enzyme called tyrosine hydroxylase (TH). In the second step, the amino acid decarboxylase enzyme (AADC) quickly converts levodopa into dopamine. This newly formed dopamine is then accepted by the neighboring neuron called the postsynaptic neuron, which carries receptors for dopamine.
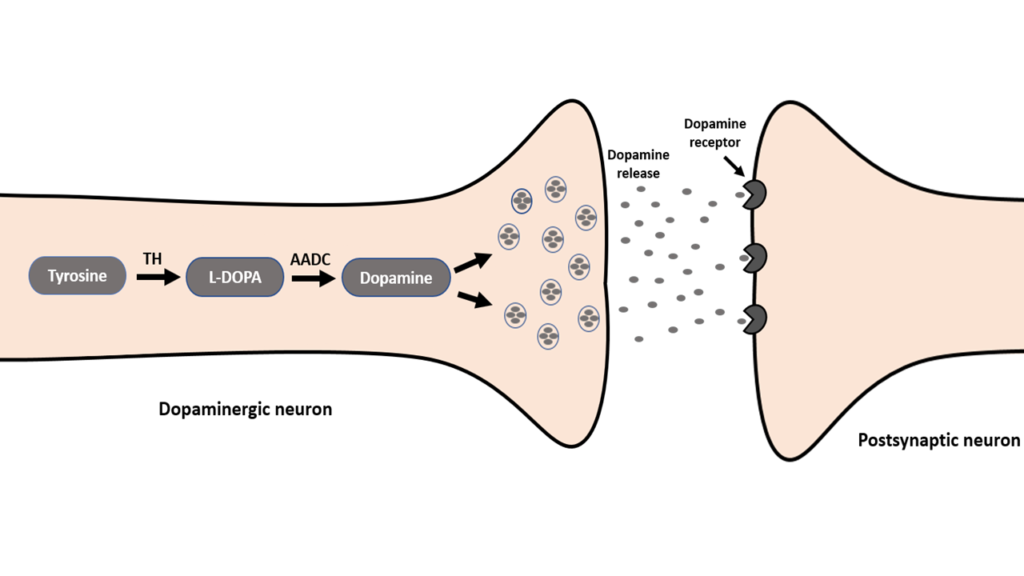
It should be noted that the postsynaptic neuron accepts not all released dopamine. The excess dopamine is either taken back by the dopaminergic neuron or it’s metabolized by two enzymes, namely the monoamine oxidase (MAO-B) and catechol-O-methyltransferase (COMT). These enzymes are located in the neighboring glial cells, which are non-neuronal cells that provide support to neurons.
So now that we know how dopamine is synthesized inside the brain, let’s look at the different classes of antiparkinsonian drugs and understand how they cause their action to reinstate the dopamine level in the brain of a Parkinson’s patient.
Levodopa
Levodopa is the most commonly used antiparkinson’s drug and is often prescribed at the early stage of the disease. It is the precursor of dopamine and efficiently converts into dopamine inside the brain.
But the question arises why to use this precursor instead of dopamine itself. And the answer is because of the blood-brain barrier. This barrier is made up of blood cells that are firmly packed together and inhibit the access of harmful substances to the brain.
Dopamine is unable to cross the blood-brain barrier while levodopa has the ability to do so. However, the problem with levodopa is that it’s susceptible to breakdown before reaching the blood-brain barrier. And because of this reason, it is often used with another drug called carbidopa. This combination allows levodopa to easily cross the blood barrier without being degraded in the periphery.
Following are the main drugs of this class:
- Sinemet
- Rytary
- Duopa
- Parcopa
These drugs may cause a number of side effects, including dizziness, constipation, diarrhea, dry mouth, loss of appetite, confusion, and weakness. The long-term use of levodopa also causes a sudden uncontrolled involuntary movement.
MAO-B and COMT Inhibitors
Levodopa helps to produce dopamine inside the brain. But the newly synthesized dopamine is susceptible to the degradative action of enzymes in the brain. This is where the two classes of drugs namely MOA-B and COMT inhibitors come into play. As the name suggests, these drugs inhibit the ability of MAO-B and COMT enzymes to degrade dopamine.
The use of MAO-B and COMT inhibitors increases the level of dopamine up to 70% in the brain and therefore very effective in controlling the motor symptoms of PD. They are often prescribed when the patient’s symptoms are not controlled with levodopa/carbidopa.
It should be noted that COMT inhibitors are also able to prevent the breaking down of levodopa outside the brain, that is in the blood. By doing so, it allows levodopa to enter the brain without being broken down.
Examples of MAO-B inhibitors include:
- Selegiline
- Rasagiline
- Safinamide
Examples of COMT inhibitors include:
- Entacapone
- Tolcapone
- Opicapone
The most common side effects of these drugs include nausea diarrhea, constipation, confusion, hallucination, sleeping problem, and vomiting.
Dopamine Agonists
This class of drugs mimics dopamine and directly stimulates dopamine receptors on the postsynaptic neuron. To put it simply, dopamine agonists act like dopamine in the brain.
Dopamine agonists are usually prescribed when levodopa is unable to control the motor symptoms of PD. Unlike levodopa, they do not need the help of other transporters to reach the brain.
Following are examples of this class of drug:
- Pramipexole
- Bromocriptine
- Ropinirole
- Pergolide
- Apomorphine
- Rotigotine
Patients using dopamine agonists may experience mental disturbance, hallucination, and confusion. These side effects are common in old patients.
Muscarinic Receptors Antagonists
In PD, there is an imbalance between dopamine and acetylcholine, another well-known neurotransmitter in the brain. While dopamine is depleted in PD, there is an increased level of acetylcholine. This imbalance causes the hyperactivity of muscarinic receptors located on the neurons responsible for motor control. As a result, the patient experiences symptoms like tremor and rigidity.
Here, the use of muscarinic receptor antagonists is more effective. They act by blocking the muscarinic receptors and decreasing the levels of acetylcholine. This helps to recover the balance between dopamine and acetylcholine, resulting in alleviating the tremor and rigidity symptoms.
Examples of this class of drugs include:
- Benztropine
- Trihexyphenidyl
- Biperiden
- Procyclidine
The most common side effects that can occur with the use of muscarinic receptor antagonists include constipation, urinary retention, dry mouth, and dementia.
Amantadine
Amantadine is distinctly different from all of the above-mentioned classes of drugs. It is available in different forms with the brand-name drug Gocovri.
Amantadine is useful in treating the rigidity and slowness of movement, especially in the early stage of the disease. It could also improve excessive shaking of hands caused by the prolonged use of levodopa. It is still unknown how exactly amantadine causes these beneficial effects. One proposed mechanism is that it could facilitate dopamine release by inhibiting its reuptake and blocking glutamine receptors.
Side effects of amantadine include constipation, insomnia, agitation, hallucination, and dizziness.
Disclaimer: The information shared here should not be taken as medical advice. The opinions presented here are not intended to treat any health conditions. For your specific medical problem, consult with your health care provider.
