Mornings can be the hardest part of the day for many people living with Parkinson’s disease. Stiffness, slowness, tremor, and delayed medication effects often collide all at once, making even simple tasks feel overwhelming. A well-designed Parkinson’s morning routine can help calm the nervous system, ease movement, and prevent symptoms from escalating — not by rushing, but by working with how the Parkinson’s brain functions in the early hours.
Mornings with Parkinson’s disease can feel unpredictable and exhausting before the day has even begun. Simple actions like getting out of bed, standing up, or walking to the bathroom may require far more effort than expected. For many people, mornings set the tone for the entire day — and when they start poorly, symptoms often escalate.
Mornings don’t have to be endured or rushed through. With the right approach, they can become more manageable, calmer, and even supportive of better movement later in the day. A well-designed Parkinson’s morning routine works with the nervous system rather than against it, helping ease stiffness, reduce stress, and prepare the body for movement.
What this article is about
This article provides a practical, realistic guide to mornings with Parkinson’s disease, based on current research and clinical experience.
You’ll learn:
- Why Parkinson’s symptoms are often worse in the morning
- How overnight changes in the brain affect movement and medication response
- What a Parkinson’s-friendly morning routine actually looks like
- Which common morning habits make symptoms worse — and why
- How to adapt your routine for different energy levels and symptom patterns
Rather than offering generic advice, this guide focuses on small, intentional changes that can make mornings feel less overwhelming and more predictable.
Why mornings are so hard with Parkinson’s disease
For many people living with Parkinson’s disease, mornings feel difficult compared to the rest of the day. This is not a lack of motivation or willpower. It reflects how Parkinson’s disease affects the brain and body after hours of rest.
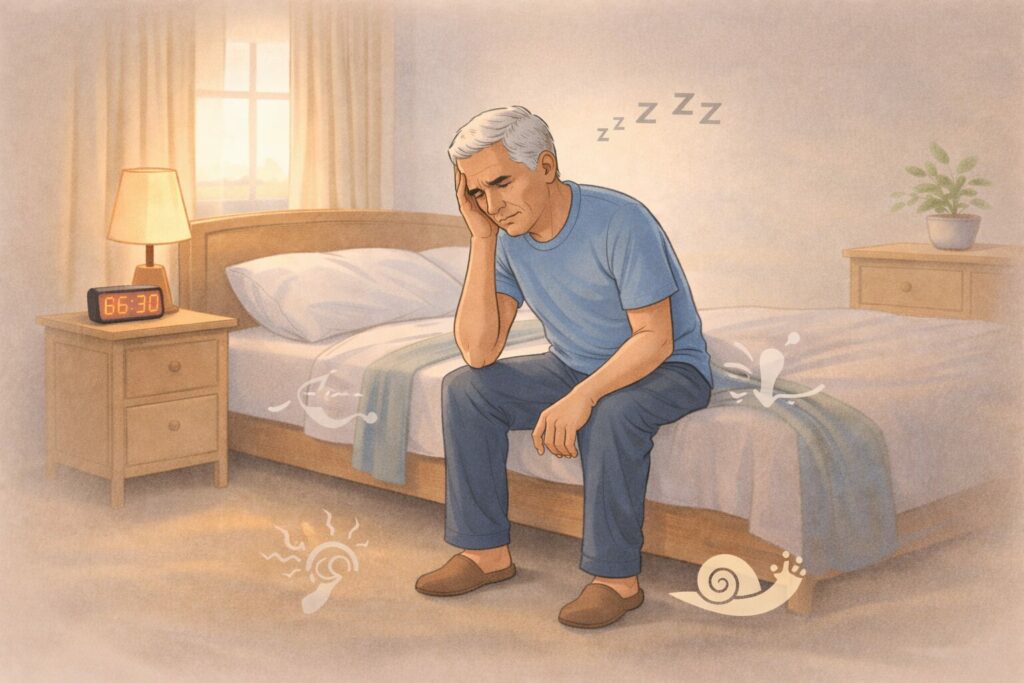
Overnight, dopamine levels naturally drop. By morning, many people wake in a pronounced OFF state, where medication from the previous day has worn off, and the nervous system is slower to initiate movement. This contributes to the familiar combination of stiffness, slowness (bradykinesia), tremor, and sometimes freezing right after waking.
Muscles also tend to feel tighter in the morning, but this stiffness is not purely muscular. In Parkinson’s disease, rigidity is driven by altered brain signaling, which means stretching or forcing movement too quickly often backfires. Instead of loosening up, the body may feel more resistant or shaky.
Another challenge is sleep inertia, the brain’s gradual transition from sleep to full alertness. Parkinson’s disease can amplify this effect, making coordination and balance less reliable in the first hour of the day. This is one reason why falls and freezing episodes are more likely in the morning.
Medication timing adds another layer. Morning doses may take longer to absorb due to slower gut motility, which is common in Parkinson’s disease. During this gap, symptoms can feel at their worst, especially if the morning is rushed or stressful.
Perhaps most importantly, mornings often come with time pressure. The expectation to get up, get dressed, and “get going” quickly places cognitive and emotional strain on an already vulnerable system. Stress and urgency further worsen motor symptoms, creating a cycle where the harder someone tries to push through the morning, the harder it becomes.
Understanding why mornings are difficult is the first step toward changing them. A Parkinson’s-friendly morning routine is not about doing more; it’s about doing the right things in the right order, at a pace that supports the nervous system rather than overwhelming it.
In the next section, we’ll look at what actually happens in the Parkinson’s brain overnight — and why that knowledge changes how mornings should be approached.
What happens in the Parkinson’s brain overnight

To understand why mornings feel so different with Parkinson’s disease, it helps to look at what happens in the brain and body during sleep.
Overnight, dopamine levels steadily decline. For people with Parkinson’s disease, this drop is more noticeable because dopamine reserves are already limited. By the time you wake up, the brain’s motor circuits are often operating at their lowest point of the day. This is why many people experience a pronounced morning OFF state, even before the first dose of medication has had a chance to work.
At the same time, the brain shifts out of sleep mode gradually. This process—sometimes called sleep inertia—affects attention, coordination, and balance. In Parkinson’s disease, this transition can be slower and less smooth, making movements feel heavy, delayed, or poorly coordinated in the early morning.
Rigidity and stiffness also tend to increase overnight. Importantly, this stiffness is not just about muscles being inactive. In Parkinson’s disease, rigidity is driven by altered signaling between the brain and muscles. That’s why aggressive stretching or forcing movement immediately after waking often feels ineffective or uncomfortable. The nervous system needs time and gentle input to “re-engage” normal movement patterns.
Another factor is medication absorption. Gastrointestinal motility is often slower in Parkinson’s disease, especially in the morning. This means that even after taking medication, it may take longer than expected to reach the brain. During this window, symptoms can temporarily feel worse, which can be frustrating if the morning is rushed.
Finally, stress plays a significant role. The brain in Parkinson’s disease is particularly sensitive to pressure and urgency. Feeling rushed first thing in the morning increases cognitive load and can amplify stiffness, tremor, and freezing. This creates a cycle where anxiety about the morning actually makes symptoms harder to manage.
Taken together, these overnight changes explain why mornings require a different strategy. They also explain why a Parkinson’s-friendly morning routine focuses on calm sequencing, gentle activation, and patience, rather than speed or productivity.
In the next section, we’ll look at the core principles that make a morning routine genuinely helpful for Parkinson’s disease — and why doing less, but in the right order, often leads to better days.
Core principles of a Parkinson’s morning routine (2026 Update)
A helpful morning routine for Parkinson’s disease is not about discipline, speed, or “pushing through.” Research and clinical practice agree that mornings require a different set of rules than the rest of the day.
These core principles form the foundation of a routine that actually helps.
Start slow to move better later
In Parkinson’s disease, the nervous system needs time to transition from rest to movement. Rushing early in the morning increases stiffness, freezing, and imbalance. Starting slowly allows motor circuits to activate gradually, reducing the likelihood that symptoms will spike.
This does not mean staying in bed indefinitely. It means choosing smooth transitions over sudden effort.
Sequence matters more than duration
A morning routine does not need to be long to be effective. What matters most is the order of activities. Breathing and gentle awareness before standing, posture and balance before walking, and light movement before more demanding tasks help the brain organize movement more efficiently.
Many people find that a short, well-sequenced routine works better than a longer, unfocused one.
Calm the nervous system before demanding movement
The Parkinson’s brain is particularly sensitive to stress. Morning anxiety, time pressure, or frustration can immediately worsen motor symptoms.
Including breathing, pauses, and moments of stillness before movement helps regulate the autonomic nervous system. A calmer nervous system responds better to movement and medication.
Consistency beats perfection
Doing the same small routine most mornings is more beneficial than attempting an ideal routine only on good days. Consistency helps the brain recognize familiar patterns, which reduces cognitive load and improves movement initiation.
Missing a day or adjusting the routine does not mean failure. Flexibility is part of success.
Adapt to the day you’re having
Parkinson’s symptoms fluctuate. A good routine allows for adjustment based on how you feel that morning. On harder days, the routine may focus only on breathing, posture, and safe transitions. On better days, it may include more movement.
A routine that adapts prevents guilt and reduces pressure — both of which help movement.
Why these principles matter
Together, these principles shift mornings from a test of endurance into a preparation phase. They reduce symptom escalation, support safer movement, and often improve how the rest of the day unfolds.
In the next section, we’ll walk through a step-by-step Parkinson’s morning routine, starting before you even get out of bed.
Step-by-step Parkinson’s morning routine

This step-by-step routine is designed to work with how Parkinson’s disease affects the brain in the early hours. It is not meant to be rushed or followed perfectly. Think of it as a framework, not a checklist.
1. Before getting out of bed
What you do in the first few minutes after waking has a powerful effect on how the rest of the morning unfolds.
Before sitting up:
- Take a few slow, steady breaths to allow the nervous system to wake gradually
- Gently move your hands, feet, or ankles to reconnect with your body
- Notice stiffness without trying to force it away
These small movements help “reboot” motor circuits before gravity, and balance demands are added.
The goal here is not exercise — it is orientation and readiness.
2. Getting out of bed safely
Transitions are often harder than movement itself in Parkinson’s disease. Getting out of bed is one of the most common moments for stiffness, hesitation, or freezing.
Helpful strategies include:
- Rolling onto your side first instead of sitting straight up
- Pausing briefly once seated to let the balance settle
- Standing up slowly, with feet placed firmly on the floor
If freezing or hesitation occurs, stopping and resetting is safer than pushing through. A calm pause often shortens the delay.
3. The first 10–20 minutes after standing
This early standing window is critical. Balance, posture, and coordination are still stabilizing, and medication may not yet be working.
During this time:
- Focus on upright posture rather than speed
- Walk slowly with deliberate steps
- Avoid multitasking, rushing, or carrying objects
Many falls and freezing episodes happen when people try to “catch up” during this phase. Slowing down here often leads to better movement later.
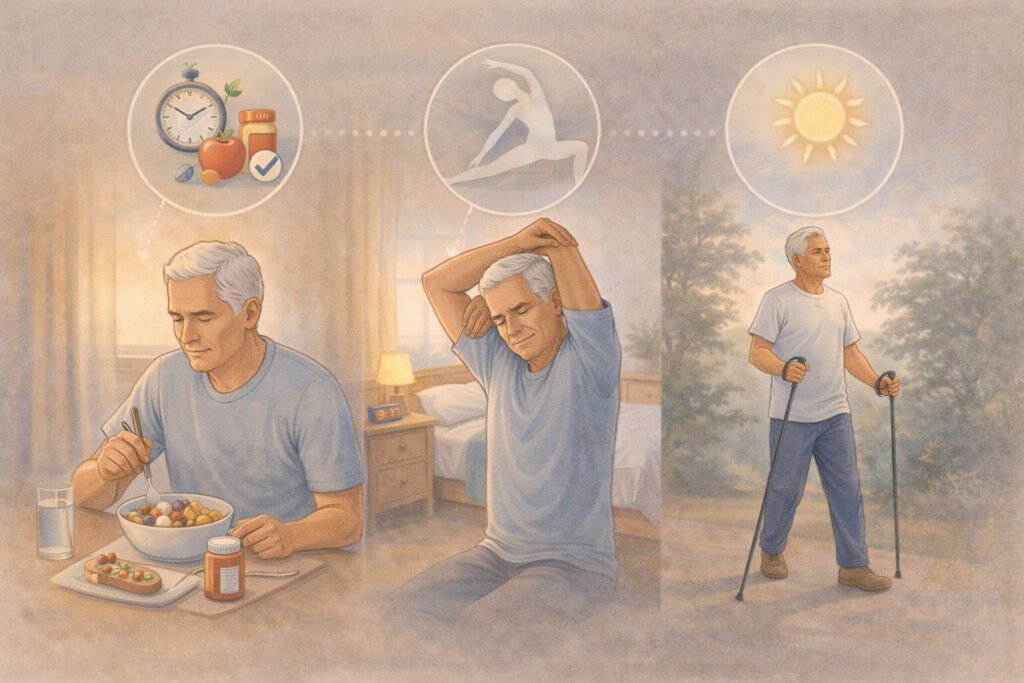
4. Coordinating movement with morning medication
Light movement can support medication absorption, but overdoing it too early may increase fatigue.
Helpful approaches include:
- Gentle walking around the home
- Simple posture and balance resets
- Avoiding strenuous exercise until medication has begun to take effect
This balance allows medication and movement to support each other, rather than compete.
5. Simple morning movements that actually help
Morning movement should focus on mobility, posture, and nervous system regulation, not intensity.
Effective options include:
- Gentle trunk and shoulder mobility
- Slow, controlled weight shifting
- Calm breathing to reduce tension
These movements prepare the body for daily activities and reduce symptom escalation, especially tremor and freezing.
Why this step-by-step approach works
Each stage builds on the one before it. Instead of demanding performance from an unready system, this routine layers readiness gradually — from awareness, to balance, to movement.
In the next section, we’ll look at how to adjust this routine for specific morning challenges, such as tremor, freezing, fatigue, or anxiety.
Morning routine adjustments for common Parkinson’s symptoms
No two mornings with Parkinson’s disease are exactly the same. Symptoms can fluctuate from day to day, and even from one morning to the next. A routine that truly helps is one that can be adjusted without guilt.
Below are simple ways to adapt the morning routine based on how you feel.
1. If tremor is worse in the morning
Morning tremor often reflects low dopamine levels combined with stress and stiffness. Trying to suppress tremor or rush through tasks usually makes it worse.
Helpful adjustments include:
- Spending a little longer on calm breathing before standing
- Moving more slowly, especially with the hands and arms
- Supporting the arms on a surface when dressing or grooming
- Prioritizing posture and relaxation over precision early on
As medication begins to work, tremor often becomes easier to manage. The goal in the early morning is containment and calm, not control.
2. If freezing happens early in the day
Freezing of gait is common in the morning due to stiffness, balance instability, and reduced attention.
Helpful adjustments include:
- Pausing before standing and before taking the first step
- Using deliberate weight shifting before walking
- Avoiding tight turns or narrow spaces immediately after getting up
- Giving yourself permission to stop, reset, and restart movement
Walking strategically in the morning is safer and more effective than trying to move “normally.”
3. If fatigue or sleepiness is high
Poor sleep, medication effects, or non-motor symptoms can make mornings feel especially heavy.
Helpful adjustments include:
- Shortening the routine to just breathing, posture, and safe transitions
- Sitting longer before standing
- Breaking tasks into smaller steps with rest in between
On low-energy mornings, doing less in the right order is far better than skipping the routine entirely.
4. If anxiety or stress is high
Anxiety strongly worsens Parkinson’s symptoms, especially first thing in the morning.
Helpful adjustments include:
- Starting with breathing before any physical movement
- Reducing time pressure wherever possible
- Preparing clothes or items the night before
- Reminding yourself that slower mornings are expected, not a failure
A calm nervous system supports better movement and better medication response.
5. If you have limited time or caregiver support
Some mornings are unavoidably rushed. On those days, focus on non-negotiables:
- One or two minutes of breathing
- A pause before standing
- Slow, deliberate first steps
Even a shortened routine can reduce symptom escalation if it respects the brain’s needs.
Key message of this section
A helpful Parkinson’s morning routine adapts to the day you’re having — not the day you wish you were having.
In the next section, we’ll look at what does not help in the morning, and why certain well-meaning habits often make symptoms worse.
What does not help in the morning (and why)
When mornings are difficult, it’s natural to want to push through and “get on with the day.” Unfortunately, some common habits often make morning symptoms worse for people living with Parkinson’s disease.
Understanding what does not help is an important part of building a routine that actually works.
Rushing through stiffness
Trying to move quickly before the nervous system is ready often increases rigidity, tremor, and imbalance. Sudden effort places extra demand on motor circuits that are still underactive in the early morning.
Slowing down early usually leads to smoother movement later.
Forcing or aggressive stretching
While stretching is often recommended, aggressive or fast stretching immediately after waking can increase discomfort. Morning rigidity in Parkinson’s disease is neurologically driven, not just muscular, so forcing range of motion rarely produces relief.
Gentle, slow movement is far more effective than pushing for flexibility.
High-intensity exercise first thing
Intense exercise too early can worsen fatigue and increase tremor or freezing, especially before medication has begun to work. Many people find that high effort early in the day leaves them depleted later on.
Morning movement should prepare the body, not exhaust it.
Multitasking while walking
Talking, carrying items, checking the phone, or rushing while walking in the morning increases cognitive load. This raises the risk of freezing, imbalance, and falls.
Early walking is safest when it is single-task and deliberate.
Skipping the morning routine altogether
On difficult mornings, it can be tempting to skip movement entirely. While rest is sometimes needed, completely avoiding gentle activation often prolongs stiffness and delays symptom improvement.
Even a shortened routine can help the nervous system transition into movement.
Key message of this section
Mornings with Parkinson’s improve when effort is replaced with intention,
and speed is replaced with sequencing.
In the next section, we’ll put everything together with a realistic sample Parkinson’s morning routine, designed for different energy levels and time constraints.
A sample Parkinson’s morning routine (realistic version)

A helpful morning routine for Parkinson’s disease does not need to look the same every day. Symptoms fluctuate, energy varies, and some mornings are simply harder than others. The routines below are meant to be adaptable, not aspirational.
Choose the version that fits the day you’re having.
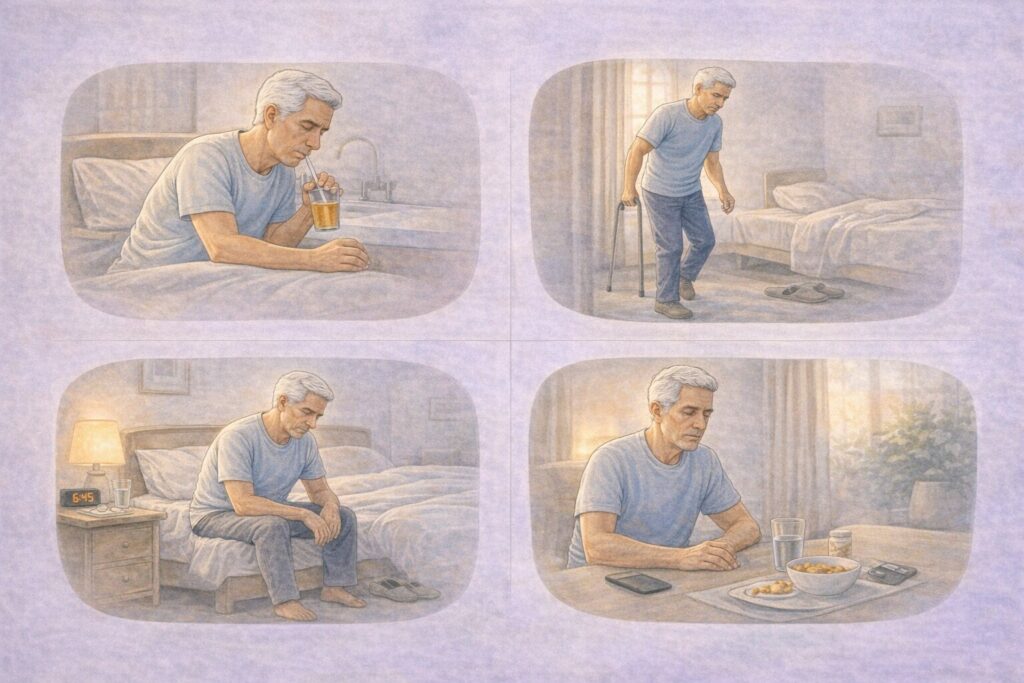
The 5-minute routine (very low energy days)
On mornings when stiffness, fatigue, or poor sleep dominate, focus only on the essentials.
- A minute of calm breathing before sitting up
- Gentle hand and foot movements in bed
- A slow transition to sitting, then standing
- Deliberate first steps, with a pause if needed
This short routine helps prevent symptom escalation without exhausting you.
The 15-minute routine (most Days)
This is the core routine for many people.
- Breathing and gentle movement before getting out of bed
- Safe, unhurried transitions to standing
- Slow walking with attention to posture
- Light mobility for shoulders, trunk, and hips
- Calm movement while medication begins to take effect
This version balances preparation and efficiency.
The 30-minute routine (good days)
On mornings when energy is better, you can build on the basics.
- Everything in the 15-minute routine
- Additional posture and balance work
- Gentle strength or resistance exercises
- Slightly longer walking periods
Even on good days, avoid rushing or pushing early.
How to adapt without guilt
A routine that truly helps is one you return to consistently. Skipping steps, shortening the routine, or needing more time does not mean failure.
The goal is not productivity — it is setting up the nervous system for the rest of the day.
Key message of this section
A successful Parkinson’s morning routine is flexible, forgiving, and built around how you feel today.
In the next section, we’ll focus on what this means for patients today, bringing the science and routines back to real-life reassurance and empowerment.
What this means for Parkinson’s patients today
Living with Parkinson’s disease often means navigating unpredictable mornings. The most important takeaway from this guide is that difficult mornings are not a personal failure — they are a reflection of how Parkinson’s affects the brain after rest.
A well-designed morning routine does not eliminate symptoms, but it can change how strongly they take hold. By slowing down early, sequencing movements thoughtfully, and reducing stress, many people find that stiffness eases sooner, balance feels more secure, and the rest of the day unfolds more smoothly.
This approach also helps shift the mindset. Instead of starting the day feeling behind, a Parkinson’s-friendly routine reframes mornings as preparation rather than performance. Even small actions — a few calm breaths, a pause before standing, or deliberate first steps — can reduce symptom escalation and improve confidence.
Perhaps most importantly, this routine is meant to be kind to yourself. Parkinson’s symptoms fluctuate, and routines should flex accordingly. Progress comes from consistency, not perfection.
Key insight
A good morning routine doesn’t make Parkinson’s disappear — it gives you a calmer, steadier start so symptoms have less control over your day.
In the final section, we’ll bring everything together with a brief conclusion and reinforce why realistic routines matter more than rigid rules.
Conclusion: Rethinking mornings with Parkinson’s disease
Mornings with Parkinson’s disease do not need to be a daily struggle or a test of endurance. As research and clinical experience increasingly show, the way the day begins can strongly influence how symptoms unfold.
A Parkinson’s morning routine that actually helps is not about doing more — it’s about doing things in the right order, at the right pace, and with an understanding of how the Parkinson’s brain functions after rest. Gentle activation, calm transitions, and reduced pressure allow the nervous system to reengage more smoothly.
These routines also offer something just as important as physical benefit: confidence. When mornings are approached with intention rather than urgency, many people feel less anxious, more stable, and better prepared to meet the day on their own terms.
Over time, small, consistent changes compound. Even when symptoms fluctuate, a flexible routine provides a steady foundation — one that supports safety, independence, and quality of life.
Disclaimer: The information shared here should not be taken as medical advice. The opinions presented here are not intended to treat any health conditions. For your specific medical problem, consult with your healthcare provider.
We’re building a simple Parkinson’s tracking app
Free during early access. Designed for daily symptom tracking without complexity.
