Tremor is one of the most recognizable and frustrating symptoms of Parkinson’s disease. For many people, Parkinson’s tremor interferes with writing, eating, dressing, and social interactions — often in ways that medication alone does not fully control.
By 2026, exercise is no longer viewed simply as supportive care for Parkinson’s disease. It is increasingly recognized as a symptom-specific intervention, particularly for tremor, helping people improve motor control, reduce fluctuation, and regain confidence in daily activities.
This article focuses on the best exercises for Parkinson’s tremor, highlighting practical, evidence-based strategies supported by current research and clinical practice.

Parkinson’s tremor differs from other tremor disorders. It is typically a rest tremor, but many people with Parkinson’s also experience tremor during posture or movement. By 2026, research clearly shows that Parkinson’s tremor is not simply a muscle problem — it reflects abnormal signaling within basal ganglia–cortical circuits, combined with altered sensory feedback and stress responsiveness.
This understanding has reshaped exercise recommendations. Instead of focusing on strengthening isolated muscles, Parkinson’s-specific exercise now aims to:
- Stabilize motor output
- Improve sensory integration
- Reduce excessive, competing motor signals
In Parkinson’s disease, movement quality and nervous system regulation matter more than effort.
How exercise influences Parkinson’s tremor physiology
In Parkinson’s disease, tremor emerges when the brain struggles to suppress unwanted movement. Exercise helps by gently retraining these control systems.
Slow, controlled Parkinson’s-specific exercises can:
- Improve inhibitory control within motor circuits
- Enhance proprioceptive feedback, which is often impaired in Parkinson’s disease
- Reduce overflow muscle activation that worsens tremor
This is why exercises involving pauses, holds, and smooth transitions are particularly valuable for Parkinson’s tremor. They give the nervous system time to recalibrate.
What exercise can — and cannot — do for Parkinson’s tremor
It is important to be realistic, especially in Parkinson’s disease.
Exercise can:
- Reduce tremor severity in many people with Parkinson’s
- Improve control during functional tasks such as eating or writing
- Decrease stress-related tremor worsening
- Help stabilize daily tremor fluctuations
Exercise cannot:
- Cure Parkinson’s disease
- Eliminate tremor completely for everyone
- Replace dopaminergic medication or medical care
In 2026, clinicians emphasize tremor management and functional improvement, rather than complete tremor suppression.
Key principles before starting Parkinson’s tremor exercises
Parkinson’s disease places unique demands on the nervous system, so exercise for tremor must be approached thoughtfully.
People with Parkinson’s diseaseoften experience:
- Fatigue
- Medication ON/OFF fluctuations
- Balance changes
For this reason, Parkinson’s-specific tremor exercise emphasizes calm, intentional movement. Rushing, holding the breath, or exercising while overstimulated can temporarily worsen tremor.
Many physiotherapists now recommend beginning Parkinson’s exercise sessions with a brief breathing or grounding exercise to help settle the nervous system before movement begins.
Best exercise categories for Parkinson’s tremor control (2026 Update)
Clinical note for readers
These exercises are designed to support tremor management in Parkinson’s disease, not to replace medical care. They can be adapted across disease stages and combined with physiotherapy guidance when available.
1. Slow resistance training for Parkinson’s disease
In Parkinson’s disease, tremor often increases with rapid or forceful movement. Slow resistance training helps counter this by promoting controlled muscle activation.
For people with Parkinson’s, slow resistance exercises:
- Improve stability during daily tasks like lifting objects
- Reduce sudden bursts of muscle activity that amplify tremor
- Support confidence in arm and hand use
The emphasis is always on slow tempo and light resistance, not muscle exhaustion.
Purpose
To reduce tremor by improving controlled muscle activation and minimizing sudden, forceful movements.
How to perform
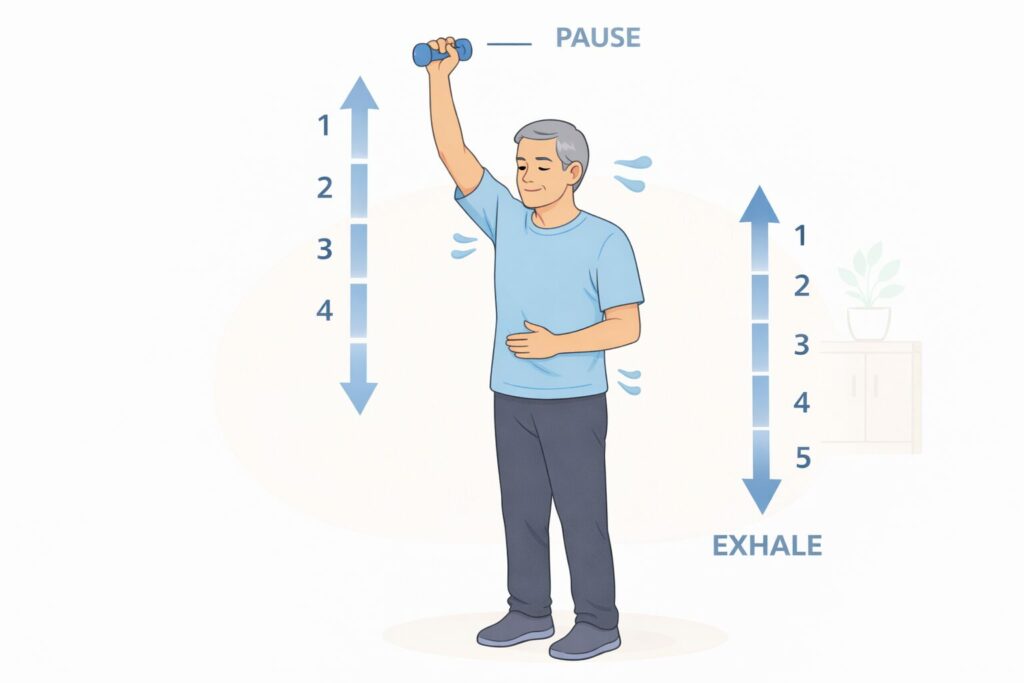
Sit or stand in a stable position. Hold a light weight or resistance band. Slowly lift your arm over 4 seconds, pause briefly, then slowly lower it over 4 seconds. Keep your breathing steady and relaxed throughout the movement.
Focus on smoothness, not strength. If tremor increases, slow down further or reduce resistance.
Key tips
- Use very light resistance
- Move as if you are “moving through thick air”
- Stop before fatigue appears
- Quality matters more than repetition count
Recommended frequency
2–4 times per week, short sessions (10–20 minutes)
2. Proprioceptive and sensory feedback exercises in Parkinson’s disease
Proprioceptive impairment is common in Parkinson’s disease. When the brain receives unclear information about limb position, it may overcorrect, increasing tremor.
Sensory-focused exercises help people with Parkinson’s disease:
- Improve awareness of arm and hand position
- Stabilize movement initiation and stopping
- Reduce tremor during precision tasks
These exercises are especially helpful for Parkinson’s tremor affecting the hands and arms.
Purpose
To improve the brain’s awareness of limb position and reduce tremor caused by overcorrection.
How to perform
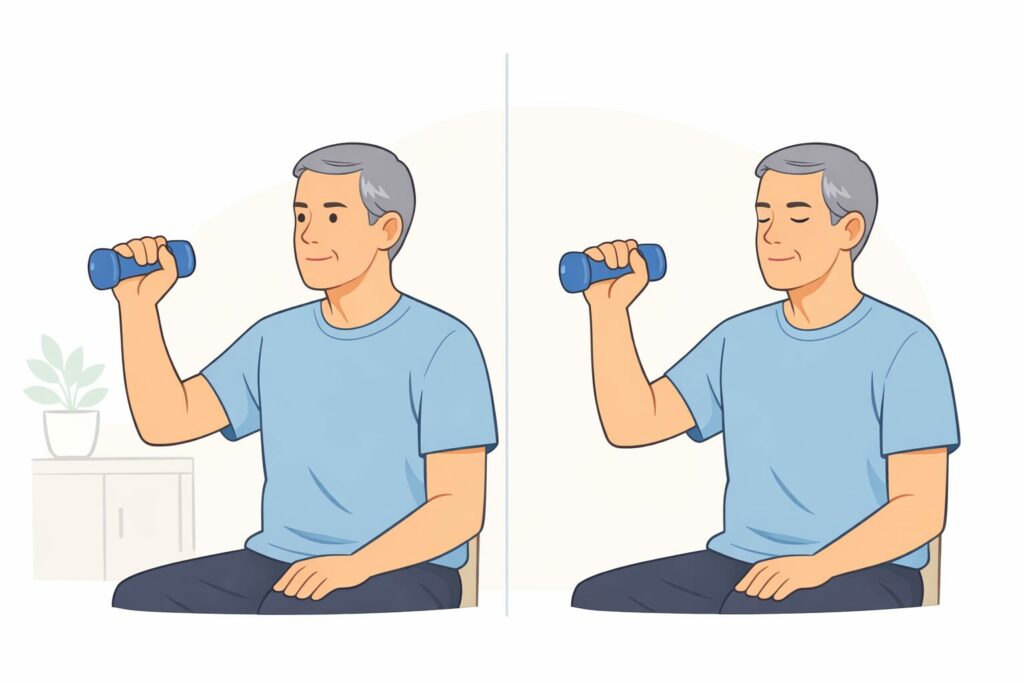
Hold a small weighted object (such as a light dumbbell or filled water bottle) in your hand. Slowly raise and lower your arm while watching the movement. Then repeat with eyes closed, focusing on how the arm feels in space.
Mirror-based exercises can also be helpful: perform slow hand movements while watching yourself in a mirror to enhance visual feedback.
Key tips
- Move slowly and deliberately
- Avoid rushing or multitasking
- Pause briefly before starting and stopping movement
Recommended frequency
Daily, especially before tasks requiring precision (eating, writing)
3. Hand and Finger Control Exercises for Parkinson’s Tremor
Hand tremor in Parkinson’s disease directly affects independence. By 2026, hand exercises for Parkinson’s focus on controlled, purposeful movement, not speed.
Practicing slow finger movements helps:
- Retrain fine motor control circuits
- Improve grip modulation
- Reduce fatigue-related tremor later in the day
Even brief daily practice can lead to meaningful functional improvements for people with Parkinson’s disease.
Purpose
To improve fine motor control, grip stability, and reduce fatigue-related tremor.
How to perform
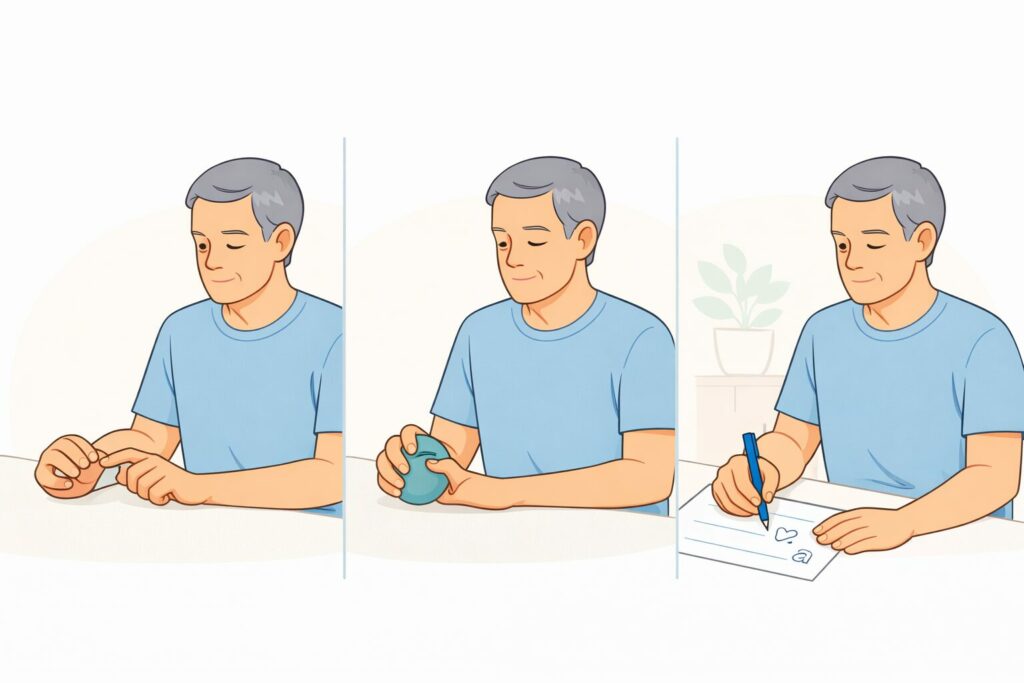
Sit comfortably with your forearm supported. Slowly touch your thumb to each finger, one at a time. Focus on accuracy rather than speed. For resistance, gently squeeze therapy putty or a soft ball, holding the squeeze for 3–5 seconds before releasing.
Slow handwriting or tracing exercises can also be included, emphasizing relaxed grip and controlled motion.
Key tips
- Keep shoulders relaxed
- Breathe steadily
- Stop if the hand feels tense or tired
Recommended frequency
Daily, even short sessions (5–10 minutes)
4. Postural stability and core control in Parkinson’s disease
Postural instability is a hallmark of Parkinson’s disease and plays a significant role in tremor severity. When the trunk is unstable, arm tremor often worsens.
Improving core and postural control:
- Creates a stable base for arm and hand movement
- Reduces compensatory tension in the shoulders and neck
- Supports smoother, more controlled motion
These exercises are usually gentle and adaptable, making them suitable across Parkinson’s stages of Parkinson’s disease.
Purpose
To create a stable trunk, reducing compensatory arm and hand tremor.
How to perform

Sit upright on a chair with feet flat on the floor. Gently engage your abdominal muscles as if bracing for a cough, without holding your breath. Maintain this gentle activation while slowly raising and lowering one arm.
You may also practice small weight shifts or seated balance holds to improve trunk control.
Key tips
- Avoid stiff or rigid posture
- Think “tall and relaxed”
- Keep neck and shoulders loose
Recommended frequency
3–5 times per week, or daily if tolerated
5. Breathing and Autonomic Regulation in Parkinson’s Tremor
Stress, anxiety, and autonomic dysfunction are common in Parkinson’s disease and strongly influence tremor severity.
Slow breathing exercises help people with Parkinson’s by:
- Reducing sympathetic nervous system overactivity
- Lowering baseline tremor reactivity
- Improving emotional regulation
By 2026, breathing exercises are considered essential for Parkinson’s tremor management, not optional.
Purpose
To calm the nervous system and reduce stress-related tremor amplification.
How to perform

Sit comfortably. Place one hand on your chest and one on your abdomen. Slowly inhale through your nose, allowing the abdomen to rise. Exhale slowly through the nose or mouth, letting the abdomen fall.
A simple rhythm is 4 seconds in, 6 seconds out. Focus on softness and ease rather than depth.
Key tips
- Never force the breath
- Longer exhales are more calming
- Practice before stressful activities
Recommended frequency
Daily and anytime tremor worsens due to stress or anxiety
Conclusion: Parkinson’s tremor management in 2026
In 2026, Parkinson’s tremor is understood as a network-level problem, shaped by movement quality, sensory feedback, posture, and emotional state. Exercise has become a core tool for managing this complexity.
For people living with Parkinson’s disease, tremor-focused exercise offers a practical way to:
- Regain a sense of control
- Improve daily function
- Reduce symptom unpredictability
While exercise does not cure Parkinson’s disease, it empowers people to work with their nervous system — one calm, intentional movement at a time.
We’re building a simple Parkinson’s tracking app
Free during early access. Designed for daily symptom tracking without complexity.
